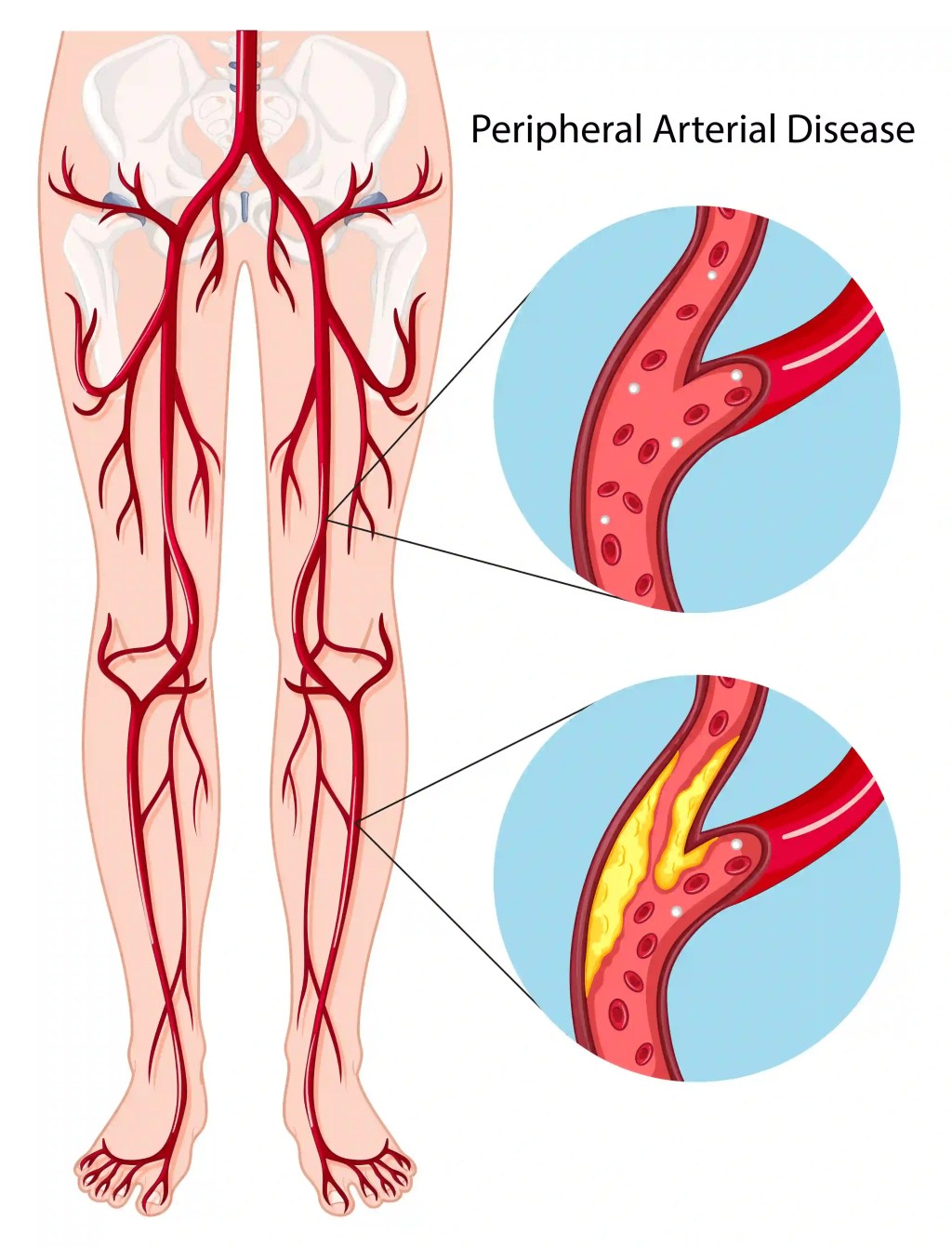
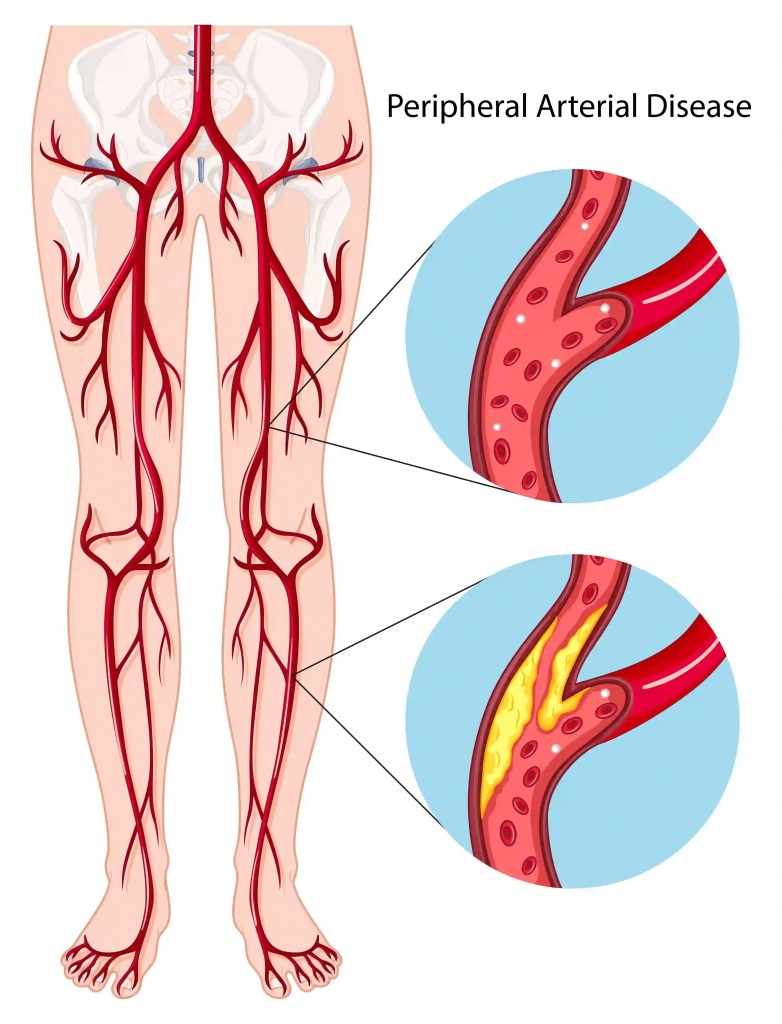
Peripheral Arterial Disease (PAD) is a circulatory condition that occurs when arteries become narrowed or blocked due to plaque buildup, restricting blood flow to the limbs. Understanding the risk factors that contribute to PAD is critical for prevention, early diagnosis, and effective treatment.
In the UAE, lifestyle-related health conditions such as diabetes, high cholesterol, and hypertension are prevalent, contributing to increased awareness and diagnoses of PAD.

Why Risk Factors Matter
Risk factors don’t just raise your chances of developing PAD—they can influence how quickly the condition progresses and how severe the symptoms become. Identifying and addressing these factors early can delay onset, reduce complications, and improve overall vascular health.
Major Risk Factors for PAD
Below are the most significant contributors to PAD, many of which are common and preventable:
- Diabetes: Chronic high blood sugar can damage blood vessels and impair circulation.
- Smoking: Tobacco use accelerates arterial damage and increases the likelihood of blood clots.
- High Blood Pressure (Hypertension): Over time, increased pressure weakens arterial walls.
- High Cholesterol: Excess cholesterol leads to plaque buildup inside arteries.
- Obesity: Excess weight contributes to hypertension, diabetes, and sedentary habits.
- Age Over 50: Risk increases with age, particularly when combined with other conditions.
- Family History of Vascular Disease: A genetic predisposition can raise your risk.
Diagnosing PAD in At-Risk Individuals
Early detection in high-risk individuals is key. Doppler ultrasound, and ankle-brachial index (ABI) test are very useful as initial tests to determine the presence of PAD.
Reducing Your Risk: Lifestyle Modifications That Work
Making the following changes can significantly reduce your PAD risk:
- Stop smoking completely
- Manage diabetes through diet, exercise, and medication
- Keep cholesterol and blood pressure under control
- Eat a balanced, heart-healthy diet
- Incorporate regular walking or low-impact aerobic activity
When to See a Specialist
If you fall into one or more of the high-risk categories listed above, it’s important to consult a vascular specialist even if symptoms are mild or absent. Early PAD can be silent but may progress to serious complications like ulcers, gangrene, or limb loss.
What to do if you are in the UAE / Dubai
Risk factor management and early intervention are central to PAD care. In Dubai, consultants such as Dr. Soroush Sohrabi, a UK-trained vascular surgeon, provides tailored assessments and minimally invasive treatments for patients at risk. His approach is rooted in evidence-based care, international fellowship training, and patient education.
Book a Vascular Risk Assessment
If you are concerned about your risk for PAD, early evaluation can make all the difference. Visit www.vascular-surgeon.ae to book a consultation with Dr. Soroush Sohrabi.
FAQs
Q: I have diabetes—should I be screened for PAD?
A: Yes. Diabetics are at significantly higher risk and should undergo regular vascular assessments.
Q: Does quitting smoking reduce my risk even if I smoked for years?
A: Absolutely. Quitting at any stage slows arterial damage and improves circulation.
Q: Can PAD be prevented entirely?
A: While not all cases can be prevented, managing risk factors can delay onset and reduce severity.
Q: Are PAD risk factors the same as heart disease risk factors?
A: Many are shared, including smoking, hypertension, and high cholesterol. PAD often coexists with coronary artery disease.




You must be logged in to post a comment.